Better lives for women
The operation to repair pelvic organ prolapse, most often hysterectomy and pelvic reconstruction to repair the connective tissue which has been damaged, is reliable and usually has few complications. In our experience, patients are usually up and about within 24 hours.
And the results are life changing!
Our patients have returned to work and family with their bodies restored and energy renewed. Some avert more devastating social consequences like repudiation. It allows them to continue forward.
Pelvic organ prolapse can affect
women of any age
There are a number of factors that predispose, cause and worsen pelvic organ prolapse. Not only do genetic factors and race influence the risk of prolapse but loss of support to the pelvic floor can be happen when any part of the pelvic floor is injured.
Injury can occur during vaginal delivery, surgery, pelvic radiation or with pelvic fractures from falls or accidents. In addition, constipation, chronic straining, chronic cough, heavy lifting and obesity are all condition that increase the risk of prolapse. Aging, menopause and loss of estrogen also contribute to weakening of the pelvic floor and development of prolapse.
PELVIC ORGAN PROLAPSE
Detailed information on this medical condition
What is it about?
Pelvic organ prolapse occurs when the normal support to the vagina is lost causing a dropping of the bladder, urethra, cervix, uterus or rectum. The pelvic floor includes the muscles, ligaments, connective tissue and nerves that support the uterus, vagina, rectum and bladder.
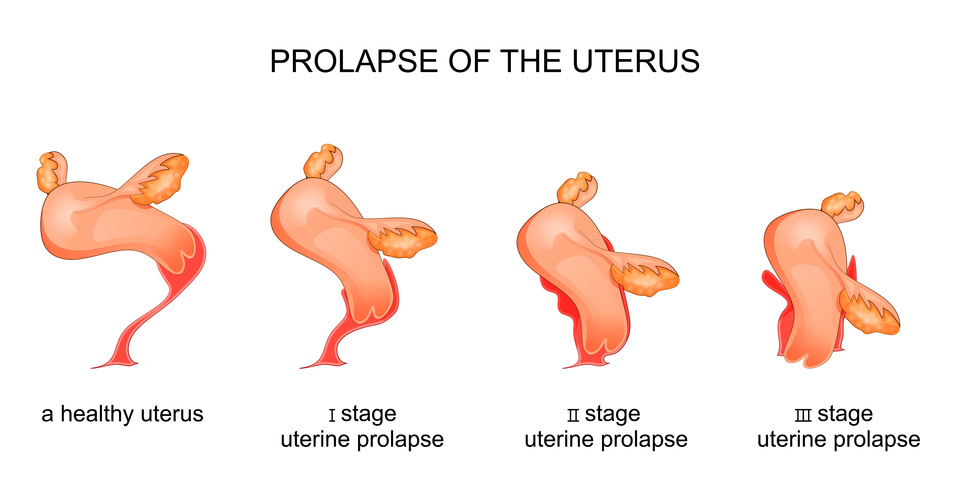
Prolapse literally means “to fall out of place”
There are several disorders and symptoms that can result from loss of support to the pelvic floor.
CHANGE A LIFE TODAY
Join us by volunteering or support us in our commitment to these women. Help us pay for their surgeries and recovery